Quality measurement in healthcare has been a complex challenge and critical priority for decades. Providers and regulatory bodies know that consistent, evidence-based metrics are key to driving real improvements in patient outcomes. That’s where CMS quality measures come in. They assess how well healthcare providers deliver care, covering everything from clinical processes and patient outcomes to hospital systems and individual experiences. CMS uses them in quality improvement programs, public reporting, value-based payment models, and to help ensure care is equitable across different populations.
This article will provide practical tips on how care providers can improve their CMS quality measures, leverage internal audits to improve care standards, and manage costs.
- Understanding CMS Quality Measures
- Types of CMS Quality Measures
- CMS Quality Measures Lifecycle: How are They Developed & Used?
- Improve Care Quality with Healthcare Compliance Software
- Free Clinical Audit Checklists to Enhance Healthcare Quality
- Importance of CMS Quality Measures
- Challenges Associated with CMS Quality Measures
- Digital Quality Measures (dQMS): An Overview
- Electronic Clinical Quality Measures (eCQMs)
Understanding CMS Quality Measures
CMS quality measures are standardized tools used to evaluate healthcare services. These measures assess processes, outcomes, patient perceptions, and healthcare structures to ensure high-quality care. They help determine whether healthcare services are safe, effective, patient-centered, timely, and efficient.
Quality measures provide a comprehensive view of healthcare quality by addressing:
- Health outcomes: The effect of healthcare interventions on patients’ health.
- Clinical processes: The effectiveness and appropriateness of medical procedures.
- Patient safety: The prevention of harm during healthcare delivery.
- Efficient use of healthcare resources: Ensuring cost-effective, appropriate care.
- Care coordination: Effective communication between providers for seamless patient care.
- Patient engagement: Encouraging patients to actively participate in their healthcare.
- Patient perceptions: Assessing patient satisfaction and experience.
- Population and public health: Measuring the impact of healthcare on broader communities.
Components of CMS Quality Measures
A CMS quality measure typically consists of:
- Title and description: Clearly defines the measure’s purpose.
- Numerator (Measure focus): Describes the target outcome, process, or event expected for the defined population.
- Denominator: Specifies the population being measured, either the entire group or a subset.
- Denominator exclusions/exceptions: Identifies cases where the measure does not apply.
- Measure period: Defines the timeframe for evaluation.
- Value sets: Uses standardized codes (ICD-10, CPT) to define clinical concepts.
👉 What is CMS Measures Inventory?
The CMS Measures Inventory is a comprehensive repository of quality measures used across Medicare and Medicaid programs. It serves as a centralized resource that enhances transparency, measures coordination, and promotes public participation in healthcare quality assessment.
This inventory includes:
- Active Measures: Currently in use across CMS reporting and payment programs.
- Retired Measures: Previously used but no longer implemented.
- Measures Under Development (MUD): Pipeline measures submitted through the Measure and Instrument Development and Support (MIDS) Resource Library. These measures are still in development and have not undergone a final determination for CMS program inclusion.
- Pre-Rulemaking Measures: Measures listed in previous Measures under Consideration (MUC) Lists. These have been approved for potential use but must undergo further pre-rulemaking and rulemaking processes before implementation.
Purpose of CMS Quality Measures
These measures serve two main purposes:
Promoting Quality and Reducing Waste
- Incentivizing high performance and discouraging poor performance through public reporting and pay-for-performance programs.
- Allowing healthcare providers to track and improve their performance over time.
Enhancing Decision-Making
Providing transparent performance data (e.g., Star Ratings) to help patients, families, and caregivers choose healthcare providers based on quality, not just cost.
Types of CMS Quality Measures
A list of CMS quality measures is used to assess and enhance healthcare services. Let’s look at the different types of quality measures CMS uses.
1. Composite Measures
Composite measures combine two or more individual metrics into a single score, offering a comprehensive assessment of healthcare quality. These measures simplify complex data and facilitate comparisons across providers and institutions by indicating multiple indicators.
2. Cost or Resource Measures
With an aim to promote cost-effective care delivery, cost or resource use measures evaluate healthcare utilization by tracking service counts (e.g., procedures, diagnoses, or encounters) and applying cost metrics. Some measures quantify usage frequency, while others apply dollar amounts, such as allowable charges, paid amounts, or standardized prices.
3. Efficiency Measures
Efficiency measures assess the relationship between healthcare costs and patient outcomes. They evaluate whether resources, such as expenditures and services, are used optimally to achieve high-quality results. These measures help identify opportunities to minimize waste while maintaining or improving patient care.
4. Intermediate Outcome Measures
Intermediate outcome measures assess the short-term effects of healthcare interventions that lead to long-term health improvements. These measures help determine whether a treatment or procedure is on track to achieve the desired clinical outcome. For example, monitoring blood pressure control in hypertension management serves as a predictor of reduced cardiovascular risk.
5. Outcome Measures
CMS outcome measures evaluate the direct impact of healthcare services on a patient’s health status, providing insight into healthcare effectiveness. They capture both desirable and adverse changes, such as mortality rates, infection rates, and functional improvements.
6. Patient-Reported Outcome-Based Performance Measures (PRO-PMs)
PRO-PMs rely on patient-reported data to assess healthcare performance and ensure healthcare assessments align with patient priorities. Patients provide information through validated tools, such as instruments, scales, or single-item measures, capturing their experiences, symptoms, and quality of life.
7. Process Measures
Process measures assess whether specific, evidence-based care steps are followed correctly. These measures have a scientific basis, ensuring that adherence to recommended protocols increases the probability of positive health outcomes. For example, timely administration of antibiotics for infections is a process measure linked to better recovery rates.
8. Structure Measures
Structure measures evaluate the capacity of a healthcare provider or organization to deliver high-quality care. These measures assess key features, such as staffing ratios, technology infrastructure, and adherence to best practices. They help determine whether an institution has the necessary resources to ensure optimal patient care.
CMS Quality Measures Lifecycle: How are They Developed & Used?
CMS follows a structured Measure Lifecycle to develop, implement, and maintain quality measures. The lifecycle of CMS quality measures consists of five key stages:
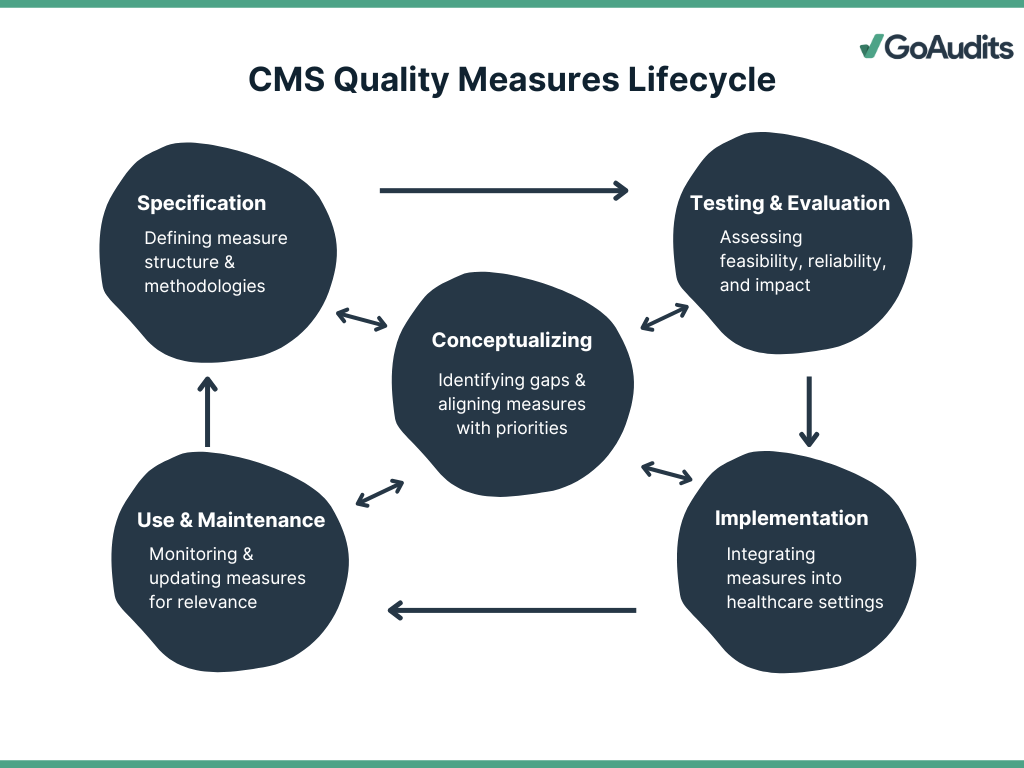
1. Conceptualizing
In this initial phase, measure developers:
- Conduct an environmental scan to identify existing gaps in healthcare quality.
- Gather input from stakeholders, including patients, caregivers, and healthcare professionals.
- Align new CMS quality measures with healthcare priorities, such as safety, efficiency, and chronic disease management.
- Narrow down broad measure concepts into specific, actionable quality measures.
2. Specification
This stage defines the measure’s structure and technical details, including:
- Target population (e.g., age groups, conditions).
- Recommended practices and interventions.
- Expected outcomes to assess quality.
- Measure calculation methodology, including performance periods and relevant medical codes.
- Harmonization with existing measures to prevent redundancy and burden.
3. Testing & Evaluation
Measures must be rigorously tested for feasibility, reliability, and impact before implementation. This phase consists of:
- Early-stage testing of measure logic, specifications, and feasibility.
- Identification of technical issues before field testing.
- Conducted in real-world healthcare settings to validate usability and scientific rigor.
- Empirical evidence is gathered to assess strengths and weaknesses.
Whether a CMS new quality measure meets the required standards is determined by four primary evaluation criteria.
- Importance: The measure must address a high-impact healthcare issue (e.g., safety, timeliness, effectiveness).
- Feasibility: The required data must be readily available and not impose an undue burden on healthcare providers.
- Scientific Acceptability: CMS new quality measure must be reliable (consistent results) and valid (accurately assesses quality of care).
- Usability & Use: It must be valuable to healthcare stakeholders (e.g., providers, policymakers, consumers) for accountability and performance improvement.
4. Implementation in different healthcare settings
Once validated, the quality measure is:
- Submitted for CMS selection and approval.
- Adopted into CMS quality reporting and payment programs.
- Implemented across various healthcare settings, such as hospitals, nursing homes, behavioral health facilities, and primary care practices.
- (Optional) Submitted for endorsement by a CMS Consensus-Based Entity (CBE).
5. Use & Maintenance
To ensure continued relevance, CMS monitors and updates measures by:
- Evaluating their impact on quality improvement programs.
- Revising or retiring measures based on advancements in clinical guidelines, data collection methods, and healthcare technology.
- Ensuring ongoing scientific soundness and effectiveness.
Improve Care Quality with Healthcare Compliance Software
Enhancing care quality in healthcare necessitates a compliance framework. GoAudits healthcare compliance software is a comprehensive solution for healthcare organizations to implement a continuous improvement cycle and ensure high standards of care and patient safety. Here’s how:
- Conduct thorough inspections up to 5 times faster with user-friendly mobile auditing tools and checklist templates tailored for different healthcare facilities.
- Attach photos, add signatures, timestamps, and geo-locations for meticulous data collection, and proactively identify and document potential issues during routine inspections.
- Upon identifying issues, assign corrective actions to specific team members, and ensure accountability by notifying assignees of their tasks, priorities, and deadlines.
- Automatically generate detailed, professional reports at the conclusion of each inspection. Customize these reports to align with your organization’s branding and promptly share them with relevant team members for review and action.
- Gain a comprehensive overview of audit performance scores across various locations, teams, or topics, with smart dashboards, allowing for immediate visibility into performance metrics.
GoAudits helps you establish a culture of continuous improvement within your organization by identifying issues, assigning and tracking corrective actions, and providing real-time insights. It not only enhances accountability but also ensures that quality and compliance standards are consistently met, leading to improved patient care.
Free Clinical Audit Checklists to Enhance Healthcare Quality
GoAudits offers the following clinical audit checklists tailored to different healthcare settings. You can sign up for free and start using these checklists to improve care standards and patient outcomes.
- Nursing Audit Checklist
- Nursing Home Safety Checklist
- Nursing Home Rounds Checklist
- Hospital Cleaning Checklist
- Patient Care Checklist
- Patient Satisfaction Survey Template
- Patient Fall Risk Assessment
- QAPI Plan Template
- QAPI Self Assessment Tool
- Home Health QAPI Readiness Template
Importance of CMS Quality Measures
The CMS quality measures significantly influence patient care by emphasizing patient-centered approaches, enhancing outcomes, fostering accountability and transparency, providing financial incentives, and driving quality improvement initiatives.
- Data Points for QAPI Plans & Programs
CMS quality measures and the framework of Quality Assurance and Performance Improvement (QAPI) are closely linked in driving healthcare quality.
CMS has identified five essential elements for developing and implementing effective, well-structured QAPI plans in any healthcare facility. These elements include: design and scope, governance and leadership, feedback, data systems, and monitoring, performance improvement projects, and systematic analysis and action. Though CMS mandates QAPI for nursing homes, implementing a QAPI plan can also be beneficial for other healthcare facilities, including home health agencies, hospices, etc.
CMS quality measures are used to evaluate outcomes and processes and assess the overall quality of healthcare provided, providing essential data for quality assessment. QAPI, on the other hand, integrates quality assurance (QA) and performance improvement (PI) into a unified, systematic approach. It also uses quality measures to identify areas for improvement and implement strategies to enhance the overall quality of care. QA focuses on maintaining established standards of care, while PI aims for continuous enhancement of healthcare processes. Essentially, CMS quality measures are the data points that inform the QAPI plans and programs, ensuring better healthcare outcomes.
- Patient-Centered Care
CMS’s Meaningful Measures Initiative underscores the importance of patient-centered care. By focusing on high-impact areas that matter most to patients, such as preventive care and management of chronic conditions, CMS ensures that healthcare delivery aligns with individual patient needs and preferences. It promotes active patient engagement and shared decision-making, leading to more personalized and effective care plans.
- Improved Outcomes
Implementing CMS quality measures has been associated with improved patient outcomes. For instance, measures targeting preventive services and chronic disease management have led to increased vaccination rates and better blood pressure control, respectively. They contribute to reduced disease complications and enhanced overall health status among patients.
- Promoting Accountability and Transparency
CMS quality measures promote accountability and transparency within the healthcare system. By publicly reporting performance data, CMS enables patients to make informed choices about their care providers. It encourages healthcare organizations to maintain high standards and continually assess their performance.
- Financial Incentives
CMS aligns financial incentives with quality performance through programs that reward or penalize providers based on their adherence to established quality measures. For example, the Hospital Value-Based Purchasing Program adjusts payments to hospitals based on the quality of care they provide, incentivizing improvements in patient care processes and outcomes.
👉 What are CMS quality programs?
CMS administers several quality programs aimed at improving healthcare outcomes, ensuring patient safety, and promoting cost-effective care across the entire healthcare system. CMS quality programs establish quality standards and performance metrics for healthcare providers, encouraging improvement through payment incentives, payment reductions, and quality improvement activities. Additionally, they enhance transparency by publicly reporting performance results, allowing consumers to make informed decisions about their care.
Key CMS quality programs include the Hospital Value-Based Purchasing (VBP) Program, Hospital Readmissions Reduction Program (HRRP), Hospital-Acquired Condition (HAC) Reduction Program, Skilled Nursing Facility Quality Reporting Program (SNF QRP), Home Health Quality Reporting Program, End-Stage Renal Disease (ESRD) Quality Incentive Program, and more.
- Quality Improvement Initiatives
CMS quality measures act as benchmarks for healthcare providers, guiding quality improvement initiatives. Identifying areas needing enhancement can help providers implement targeted strategies to elevate care quality. Continuous monitoring and reporting of these measures facilitate ongoing assessment and refinement of care practices.
Challenges Associated with CMS Quality Measures
Implementing CMS quality measures presents several challenges, including the following:
- Data Quality Issues
Accurate data is essential for reliable quality assessments. Inconsistent data collection methods and fragmented healthcare information systems can lead to incomplete or erroneous data. For instance, the lack of access to comprehensive patient data has been identified as a significant obstacle in adopting value-based care models.
- Complexity of Patient Care
Healthcare involves multifaceted patient needs that are not easily captured by standardized metrics. Quality measures may fail to account for individual patient circumstances, leading to assessments that do not fully reflect the quality of care provided.
- Lack of Alignment
Discrepancies among various quality measurement programs can cause confusion and inefficiencies. The absence of standardized measures across different healthcare settings complicates efforts to improve care quality uniformly. The Meaningful Measures Initiative by CMS aims to address this by focusing on high-priority areas and reducing the reporting burden.
- Implementation and Reporting Burden
The administrative tasks associated with implementing and reporting quality measures can be overwhelming for healthcare providers. Physicians spend considerable time on these activities, diverting attention from direct patient care.
👉 A study highlighted that US physician practices spend over $15.4 billion annually on reporting quality measures, averaging 785 hours per physician each year.
- Balancing Cost and Quality
Aligning financial incentives with quality care is challenging. Efforts to control costs might inadvertently compromise care quality, while initiatives to improve quality could lead to increased expenses. Finding a balance that ensures high-quality, cost-effective care remains a complex issue.
- Inadequately Incorporating Patient Experiences
Current quality measures often emphasize clinical outcomes and may not fully capture patient experiences and satisfaction. Incorporating patient-reported outcomes is crucial for a comprehensive assessment of care quality. The CMS National Quality Strategy emphasizes the importance of patient-centered care in its framework.
Digital Quality Measures (dQMS): An Overview
Digital Quality Measures (dQMs) represent the next phase of healthcare quality assessment, leveraging standardized, interoperable digital data to enhance measurement accuracy and efficiency. CMS is driving this transition as part of its strategy to modernize quality reporting systems.
👉 dQMs use electronic data sources, including:
– Electronic Health Records (EHRs)
– Administrative claims and clinical assessment
– Case management systems
– Laboratory data from laboratory and prescription drug monitoring programs (PDMPs)
– Patient-generated information from wearable devices and patient-generated health data
– Health Information Exchange Organizations (HIEOs)
Key Domains of CMS’s Digital Transformation Strategy
To enable a seamless shift to digital measurement, CMS has identified four core domains:
- Improving Data Quality: Enhancing data completeness, accuracy, and standardization across healthcare systems.
- Advancing Technology: Implementing FHIR APIs and cloud-based solutions to facilitate seamless data exchange.
- Optimizing Data Aggregation: Enabling data harmonization across multiple sources, reducing redundancy and administrative burden.
- Aligning Data, Tools, and Measures: Ensuring consistency across quality reporting programs to streamline processes for healthcare providers.
For each domain, CMS is evolving technical components, shaping policies, and engaging stakeholders to facilitate the transition to dQMs.
Over the past decade, CMS has worked to integrate data from EHRs into quality measurement. However, challenges remain in streamlining data collection, exchange, calculation, and reporting. The transition to dQMs will occur incrementally, taking into account varying levels of readiness among providers and care settings. Adoption will be paced with the uptake of FHIR API technology.
Electronic Clinical Quality Measures (eCQMs)
Electronic Clinical Quality Measures (eCQMs) are digitally specified quality measures that use data extracted from electronic health records (EHRs) and other health IT systems to assess healthcare quality.
Like all quality measures, eCQMs evaluate healthcare processes, outcomes, and performance, helping healthcare providers improve patient care.
eCQMs belong to a broader category – digital quality measures (dQMs), which originate from structured health data transmitted via interoperable systems.
Unlike traditional quality measures, eCQMs:
- Are specified electronically to eliminate manual data abstraction.
- Pull structured data from EHRs or health IT systems during patient care, reducing the reporting burden on clinicians.
- Support real-time quality assessment and decision-making.
The lifecycle of eCQMs closely mirrors traditional quality measures, following these key phases:
- Development: Measure developers create eCQMs based on evidence-based clinical guidelines, ensuring alignment with best practices.
- Specification: The measure is electronically specified in a standard format to enable automated data extraction.
- Implementation: Healthcare providers integrate eCQMs into EHR systems to collect and report data.
- Evaluation & Refinement: Performance data is analyzed, and the measure is updated periodically to reflect changes in medical knowledge, clinical guidelines, and coding standards.
👉 CMS and other organizations use eCQMs in various quality programs, including
– Quality reporting programs (e.g., Merit-Based Incentive Payment System – MIPS).
– Value-based purchasing initiatives that tie reimbursement to quality performance.
– Accreditation and benchmarking programs by The Joint Commission, federal health agencies, and private payers.
To ensure data consistency, validity, and interoperability, eCQMs rely on industry-recognized standards, including Clinical Quality Language (CQL), Fast Healthcare Interoperability Resources (FHIR), Health Quality Measure Format (HQMF), Quality Data Model (QDM), Quality Reporting Document Architecture (QRDA).
Benefits of eCQMs
eCQMs provide multiple advantages to healthcare organizations, clinicians, and patients, including:
- Improved Accuracy: eCQMs use structured clinical data from EHRs, enabling more precise quality assessments.
- Reduced Administrative Burden: Automated data extraction eliminates the need for manual chart abstraction and reporting.
- Real-Time Data Insights: Providers can access quality data at the point of care to enhance clinical decision-making.
- Opportunities for Continuous Improvement: Healthcare organizations can use eCQMs to monitor performance and implement data-driven quality enhancements.