- Library ›
- Healthcare ›
- CDC Infection Prevention Checklist for Dental Settings
CDC Infection Prevention Checklist for Dental Settings
Administrative Measures
1. Are written infection prevention policies and procedures specific to the dental setting available, current, and based on evidence-based guidelines (e.g., CDC / Healthcare Infection Control Practices Advisory Committee [HICPAC]), regulations, or standards? Note: Policies and procedures should be appropriate for the services provided by the dental setting and should extend beyond the Occupational Safety and Health Administration (OSHA) bloodborne pathogens training
|
Photo
Comment
|
5. Does the facility have a system for early detection and management of potentially infectious persons at initial points of patient encounter? Note: The system may include taking a travel and occupational history, as appropriate, and elements described under respiratory hygiene/cough etiquette.
|
Photo
Comment
|
Infection Prevention Education And Training
1. Does DHCPr receive job- or task-specific training on infection prevention policies and procedures and the OSHA Bloodborne Pathogens Standard: • Upon hire? • Annually? • When new tasks or procedures affect the employee’s occupational exposure? • According to state or federal requirements?
|
Photo
Comment
|
Dental Health Care Personnel Safety
11. Does the facility have well-defined policies concerning contact of personnel with patients when personnel have potentially transmissible conditions, including: • Work-exclusion policies that encourage reporting of illnesses and do not penalize staff with loss of wages, benefits, or job status? • Education of personnel on the importance of prompt reporting of illness to a supervisor?
|
Photo
Comment
|
Program Evaluation
Hand Hygiene
Personal Protective Equipment (PPE)
Respiratory Hygiene / Cough Etiquette
1. Have policies and procedures been implemented to contain respiratory secretions in people who have signs and symptoms of a respiratory infection, beginning at the point of entry to the dental setting? Do these measures include: • Posting signs at entrances instructing symptomatic patients to cover their mouths/noses when coughing or sneezing, use and dispose of tissues, and perform hand hygiene? • Providing tissues and no-touch receptacles for tissue disposal? • Providing resources for patients to perform hand hygiene in or near waiting areas? • Offering face masks to coughing patients and other symptomatic persons upon entry to the setting? • Providing space and encouraging symptomatic persons to sit as far away from others as possible (if feasible, using a separate waiting area)?
|
Photo
Comment
|
Sharps Safety
Safe Injection Practices
Sterilization And Disinfection Of Patient-Care Items And Devices
Environmental Infection Prevention And Control
Dental Unit Water Quality
Hand Hygiene Is Performed Correctly
1. Is hand hygiene performed in the following situations: • When hands are visibly soiled? • After barehanded touching of instruments, equipment, materials, and other objects likely to be contaminated by blood, saliva, or respiratory secretions? • Before and after treating each patient? • Before putting on gloves? • Immediately after removing gloves? • Before putting on a sterile surgeon’s gloves for all surgical procedures?
|
Photo
Comment
|
Personal Protective Equipment (PPE) Is Used Correctly
Protective Clothing
Respiratory Hygiene/Cough Etiquette
Sharps Safety
Safe Injection Practices
8. When using multidose vials: • Are they dedicated to individual patients whenever possible? • Are multidose vials used for more than one patient kept in a centralized medication area and not brought into the immediate patient treatment area? • Are multidose vials dated when first opened and discarded within 28 days unless the manufacturer specifies otherwise?
|
Photo
Comment
|
Sterilization And Disinfection Of Patient-Care Items And Devices
19. If digital radiography is used: • Are FDA-cleared barriers used to cover the sensor and changed between patients? • After barrier removal, is the sensor cleaned and sterilized/disinfected per manufacturer instructions, or at a minimum, cleaned and disinfected with an intermediate-level EPA-registered hospital disinfectant?
|
Photo
Comment
|
Environmental Infection Prevention And Control
Dental Unit Water Quality
Is this sample what you are looking for?
Sign up to use & customise this template, or create your own custom checklist:
Checklist by GoAudits.com – Please note that this checklist is intended as an example. We do not guarantee compliance with the laws applicable to your territory or industry. You should seek professional advice to determine how this checklist should be adapted to your workplace or jurisdiction.
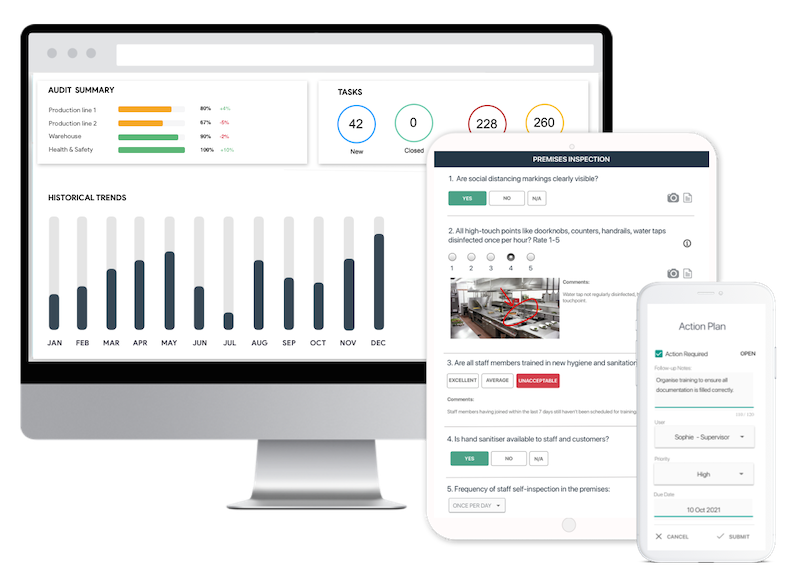
Easy inspection app for your digital checklists
- Conduct inspections anytime, anywhere - even offline
- Capture photos as proof of compliance or areas needing attention
- Instantly generate and share detailed reports after the inspections
- Assign & track follow-up tasks, view historical trends on a centralized dashboard